In a first, gene-edited cell therapy cures aggressive blood cancer
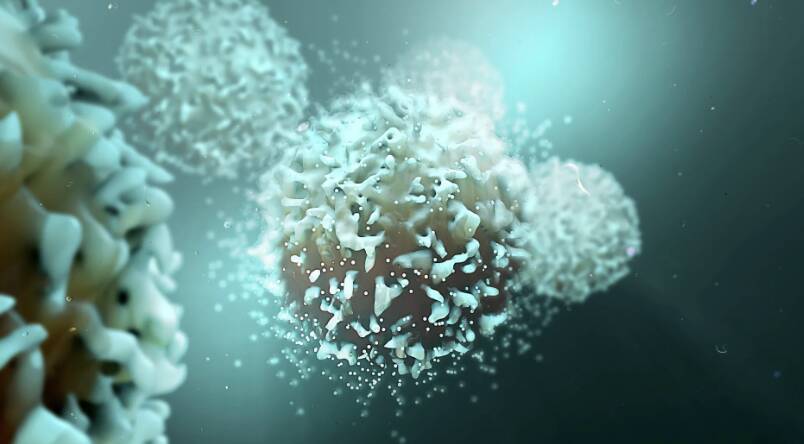
In a groundbreaking medical breakthrough, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, has shown remarkable promise in targeting and destroying cancer cells, offering new hope to patients diagnosed with this devastating disease.
T-cell acute lymphoblastic leukaemia (T-ALL) is a rare and aggressive form of blood cancer that affects the T-cells, a type of white blood cell that plays a crucial role in the immune system. Despite advances in treatment options, T-ALL remains a challenging disease to treat, with limited therapeutic options available for patients who do not respond to traditional therapies.
The BE-CAR7 therapy involves modifying immune cells, specifically T-cells, to have chimeric antigen receptors (CARs) on their surface. These CARs are engineered to recognize and target a specific protein on the surface of cancer cells, known as CD7. When the T-cell with the CAR comes into contact with a cancer cell expressing CD7, it attaches to the cell and destroys it, thereby eliminating the cancerous cells from the body.
The use of gene-edited immune cells to treat cancer is a rapidly evolving field, with several clinical trials currently underway to investigate the safety and efficacy of this approach. The BE-CAR7 therapy is a significant advancement in this field, as it has shown remarkable success in targeting and destroying T-ALL cancer cells in patients who have failed to respond to traditional therapies.
The BE-CAR7 therapy involves several steps. First, T-cells are collected from the patient’s blood and genetically modified to express the CARs on their surface. The modified T-cells are then expanded in number and infused back into the patient’s body, where they can recognize and target the cancer cells. The CARs on the surface of the T-cells bind to the CD7 protein on the cancer cells, triggering the T-cells to attack and destroy the cancerous cells.
The results of the clinical trial have been impressive, with several patients experiencing complete remission of their disease. The therapy has been well-tolerated, with minimal side effects reported. The researchers believe that the BE-CAR7 therapy has the potential to revolutionize the treatment of T-ALL and other aggressive blood cancers, offering new hope to patients who have limited treatment options available.
The success of the BE-CAR7 therapy is a testament to the power of gene editing technologies, such as CRISPR/Cas9, which have enabled scientists to precisely modify the genes of immune cells to create targeted therapies. The use of gene-edited immune cells to treat cancer is a rapidly evolving field, with several clinical trials currently underway to investigate the safety and efficacy of this approach.
The implications of this breakthrough are significant, as it has the potential to transform the treatment of aggressive blood cancers. The BE-CAR7 therapy offers a new and innovative approach to targeting cancer cells, one that is more precise and effective than traditional therapies. The researchers believe that this therapy could be used to treat a range of blood cancers, including leukaemia, lymphoma, and myeloma.
In conclusion, the success of the BE-CAR7 therapy in treating T-cell acute lymphoblastic leukaemia is a groundbreaking medical breakthrough that offers new hope to patients diagnosed with this aggressive blood cancer. The use of gene-edited immune cells to target and destroy cancer cells is a rapidly evolving field, one that has the potential to revolutionize the treatment of cancer. As researchers continue to explore the potential of this approach, we can expect to see significant advances in the treatment of blood cancers and other diseases.
News source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm