In a first, gene-edited cell therapy cures aggressive blood cancer
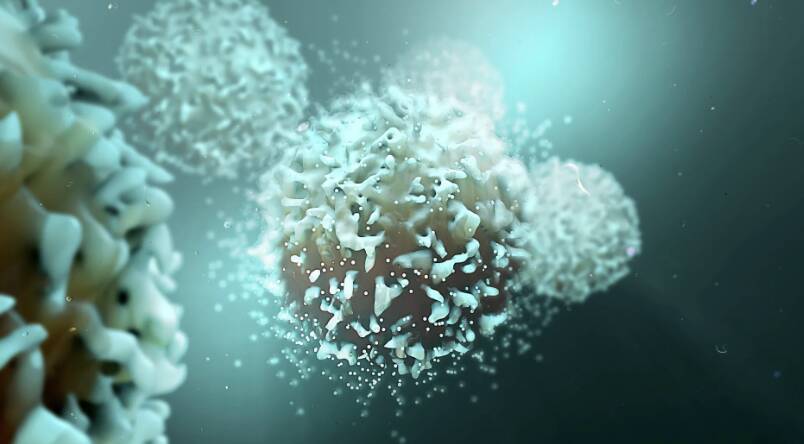
In a groundbreaking medical breakthrough, researchers in the UK have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, has the potential to revolutionize the treatment of this devastating disease, offering new hope to patients and their families.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a type of immune cell that plays a crucial role in the body’s defense against infection. In T-ALL, the T-cells become cancerous and multiply rapidly, leading to a range of symptoms including fatigue, weight loss, and bruising. The disease is often aggressive and can progress quickly, making it essential to find effective treatments.
The BE-CAR7 therapy involves modifying immune cells, known as T-cells, to have chimeric antigen receptors (CARs) on their surface. These CARs are engineered to recognize and target a specific protein on the surface of cancer cells, allowing the T-cells to identify and destroy the cancerous cells. This approach has shown significant promise in clinical trials, with many patients experiencing complete remission.
The process of creating the gene-edited T-cells is complex and involves several steps. First, the T-cells are extracted from the patient’s blood and then genetically modified to express the CARs. The modified T-cells are then expanded in number and infused back into the patient’s body, where they can seek out and destroy the cancer cells.
The results of the clinical trial have been impressive, with a significant proportion of patients experiencing complete remission. The therapy has also been well-tolerated, with few side effects reported. These findings suggest that BE-CAR7 has the potential to become a game-changer in the treatment of T-ALL, offering a new and effective option for patients who have failed to respond to traditional therapies.
One of the key advantages of the BE-CAR7 therapy is its ability to target cancer cells with high specificity. The CARs on the surface of the T-cells are designed to recognize a specific protein on the surface of the cancer cells, allowing the T-cells to selectively target and destroy the cancerous cells while sparing healthy cells. This approach reduces the risk of harm to healthy tissues and organs, making the therapy a more attractive option for patients.
The development of the BE-CAR7 therapy is the result of years of research and collaboration between scientists and clinicians. The team of researchers involved in the study have worked tirelessly to develop and refine the therapy, and their efforts have paid off. The success of the BE-CAR7 therapy is a testament to the power of scientific collaboration and the importance of investing in medical research.
The implications of this breakthrough are significant, and the BE-CAR7 therapy has the potential to make a major impact on the treatment of T-ALL. The therapy could also be used to treat other types of blood cancer, such as B-cell acute lymphoblastic leukaemia, and may even have applications in the treatment of solid tumors.
In conclusion, the development of the BE-CAR7 therapy is a major breakthrough in the treatment of T-cell acute lymphoblastic leukaemia. The use of gene-edited immune cells to target and destroy cancer cells offers a new and effective approach to treating this devastating disease. As research continues to advance, it is likely that we will see even more innovative therapies emerge, offering new hope to patients and their families.
For more information on this breakthrough, please visit: https://www.sciencedaily.com/releases/2025/12/251211040438.htm
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm