In a first, gene-edited cell therapy cures aggressive blood cancer
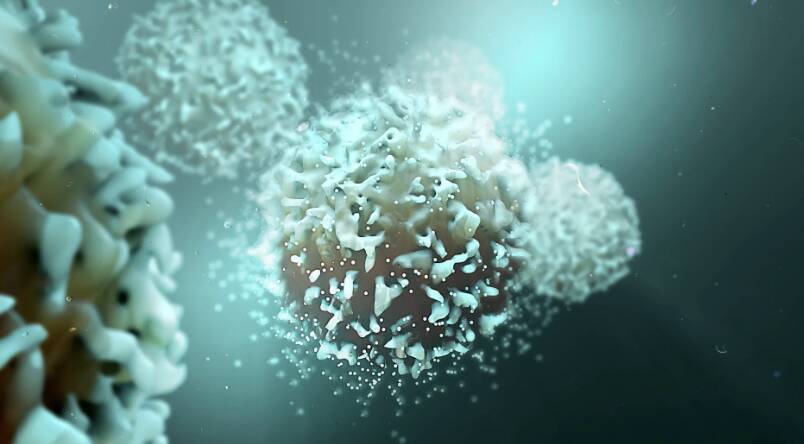
In a groundbreaking medical breakthrough, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, modifies immune cells (T-cells) to have chimeric antigen receptors (CARs) on their surface. The CARs recognize and target a specific protein on cancer cells’ surface, and the T-cell then destroys that cancer cell. This revolutionary approach has shown tremendous promise in treating this devastating disease, offering new hope to patients and their families.
T-cell acute lymphoblastic leukaemia (T-ALL) is a rare and aggressive type of blood cancer that affects the T-cells, a crucial component of the immune system. It is characterized by the uncontrolled proliferation of cancerous T-cells, which can lead to life-threatening complications if left untreated. Current treatment options for T-ALL often involve intensive chemotherapy, radiation, and bone marrow transplantation, which can have severe side effects and may not always be effective.
The BE-CAR7 therapy works by harnessing the power of the immune system to fight cancer. The gene-edited T-cells are designed to recognize a specific protein called CD7, which is present on the surface of cancerous T-cells. The CARs on the surface of the modified T-cells bind to the CD7 protein, allowing the T-cells to identify and target the cancer cells. Once the T-cells attach to the cancer cells, they release toxic chemicals that destroy the cancer cells, thereby halting the progression of the disease.
The UK researchers used a gene-editing tool called CRISPR-Cas9 to modify the T-cells and introduce the CARs. CRISPR-Cas9 is a powerful tool that allows scientists to edit genes with unprecedented precision, making it possible to develop innovative therapies like BE-CAR7. The modified T-cells were then infused into patients with T-ALL, where they began to target and destroy the cancer cells.
The results of the study were nothing short of remarkable. Patients who received the BE-CAR7 therapy experienced significant improvements in their condition, with many achieving complete remission. The therapy was also found to be relatively safe, with minimal side effects reported. These findings suggest that BE-CAR7 has the potential to revolutionize the treatment of T-ALL, offering a new and effective option for patients who have failed to respond to traditional therapies.
The success of BE-CAR7 is a testament to the power of gene editing and immunotherapy in treating cancer. By harnessing the immune system to fight cancer, researchers are developing innovative therapies that can target cancer cells with unprecedented precision. This approach has shown tremendous promise in treating a range of cancers, including leukemia, lymphoma, and solid tumors.
The implications of this breakthrough are far-reaching. For patients with T-ALL, BE-CAR7 offers a new hope for a cure. The therapy has the potential to improve treatment outcomes, reduce the risk of relapse, and enhance the quality of life for patients. Additionally, the success of BE-CAR7 paves the way for the development of similar therapies for other types of cancer, offering a new era of personalized medicine.
In conclusion, the development of BE-CAR7 is a groundbreaking achievement that has the potential to transform the treatment of T-cell acute lymphoblastic leukaemia. By using gene-edited immune cells to target cancer cells, researchers have created a powerful new tool in the fight against cancer. As this therapy continues to be developed and refined, it is likely to offer new hope to patients and their families, and pave the way for a new era of innovative cancer therapies.
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm