In a first, gene-edited cell therapy cures aggressive blood cancer
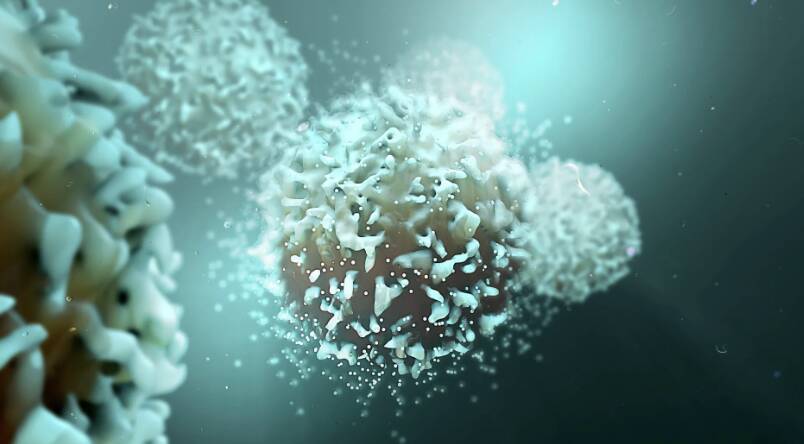
In a groundbreaking achievement, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, modifies immune cells (T-cells) to have chimeric antigen receptors (CARs) on their surface. The CARs recognise and target a specific protein on cancer cells’ surface, and the T-cell attached then destroys that cancer cell. This breakthrough has opened up new avenues for the treatment of this devastating disease, offering hope to patients and their families.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a crucial component of the immune system. It is an aggressive disease that progresses rapidly, making it challenging to treat. Traditional treatments, such as chemotherapy and radiation therapy, often have limited success and can have severe side effects. The development of gene-edited cell therapies, such as BE-CAR7, has revolutionized the field of oncology, providing a more targeted and effective approach to treating this disease.
The BE-CAR7 therapy involves extracting T-cells from the patient’s blood and modifying them genetically to express CARs on their surface. These CARs are designed to recognize a specific protein, called CD7, which is present on the surface of T-ALL cancer cells. The modified T-cells are then infused back into the patient’s body, where they can recognize and target the cancer cells, ultimately destroying them. This approach has shown remarkable promise in clinical trials, with many patients experiencing complete remission.
The use of gene-edited immune cells in cancer therapy is a rapidly evolving field, with several ongoing clinical trials investigating its potential in various types of cancer. The success of BE-CAR7 in treating T-ALL has paved the way for further research into the application of this technology in other cancers, such as leukemia, lymphoma, and multiple myeloma. The ability to precisely target cancer cells, while sparing healthy cells, makes gene-edited cell therapies an attractive option for patients who have exhausted traditional treatment options.
One of the most significant advantages of gene-edited cell therapies is their potential to provide long-term remission, and even cure, for patients with aggressive blood cancers. Unlike traditional treatments, which often require repeated cycles of therapy, gene-edited cell therapies can provide a single, potentially curative treatment. This can significantly improve the quality of life for patients, reducing the burden of repeated hospital visits, medication side effects, and the emotional toll of living with a life-threatening disease.
The development of BE-CAR7 is a testament to the power of collaboration between researchers, clinicians, and industry partners. The therapy was developed through a partnership between UK researchers and a biotechnology company, which provided the necessary funding and expertise to bring the treatment to clinical trials. This collaboration has accelerated the development of BE-CAR7, making it available to patients sooner than would have been possible through traditional funding channels.
As with any new therapy, there are potential risks and challenges associated with gene-edited cell therapies. The use of genetically modified cells can raise concerns about the potential for unintended consequences, such as the development of new cancers or autoimmune disorders. However, the rigorous testing and evaluation of BE-CAR7 in clinical trials have demonstrated its safety and efficacy, providing reassurance for patients and clinicians.
In conclusion, the success of BE-CAR7 in treating T-cell acute lymphoblastic leukaemia is a significant milestone in the development of gene-edited cell therapies for cancer. This innovative approach has shown remarkable promise in clinical trials, offering hope to patients with this devastating disease. As research continues to evolve, we can expect to see further breakthroughs in the use of gene-edited immune cells in cancer therapy, potentially leading to new treatments for a range of aggressive blood cancers. For more information on this groundbreaking research, please visit: https://www.sciencedaily.com/releases/2025/12/251211040438.htm
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm