In a first, gene-edited cell therapy cures aggressive blood cancer
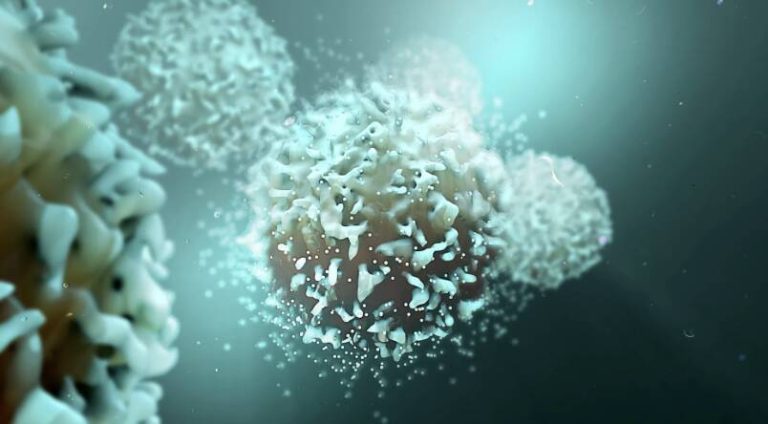
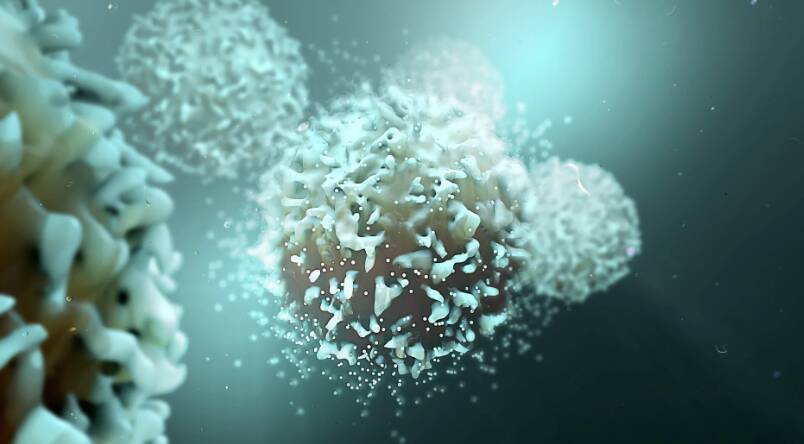
In a groundbreaking achievement, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, modifies immune cells (T-cells) to have chimeric antigen receptors (CARs) on their surface. The CARs recognize and target a specific protein on cancer cells’ surface, and the T-cell attached then destroys that cancer cell. This breakthrough has opened up new avenues for the treatment of this devastating disease and has given hope to patients and their families.
T-cell acute lymphoblastic leukaemia (T-ALL) is a rare and aggressive form of blood cancer that affects the T-cells, a type of white blood cell that plays a crucial role in the immune system. The disease is characterized by the uncontrolled proliferation of cancerous T-cells, which can lead to life-threatening complications if left untreated. Despite advancements in chemotherapy and radiation therapy, T-ALL remains a challenging disease to treat, with many patients experiencing relapses and poor outcomes.
The BE-CAR7 therapy is a type of immunotherapy, which harnesses the power of the immune system to fight cancer. The therapy involves extracting T-cells from the patient’s blood and genetically modifying them to express CARs on their surface. The CARs are designed to recognize a specific protein called CD7, which is expressed on the surface of cancerous T-cells. Once the gene-edited T-cells are infused back into the patient’s body, they can recognize and target the cancer cells, leading to their destruction.
The UK researchers used a cutting-edge gene-editing tool called CRISPR-Cas9 to modify the T-cells. CRISPR-Cas9 is a powerful technology that allows scientists to edit genes with unprecedented precision and efficiency. The tool works by cutting the DNA at a specific location, allowing researchers to insert or delete genes as needed. In this case, the researchers used CRISPR-Cas9 to insert the CAR gene into the T-cells, giving them the ability to recognize and target cancer cells.
The BE-CAR7 therapy has shown remarkable promise in clinical trials, with many patients experiencing complete remission of their disease. The therapy has also been well-tolerated, with minimal side effects reported. The researchers believe that the BE-CAR7 therapy has the potential to revolutionize the treatment of T-ALL and other types of blood cancer.
One of the most significant advantages of the BE-CAR7 therapy is its ability to target cancer cells with high specificity. Unlike traditional chemotherapy and radiation therapy, which can damage healthy cells and tissues, the BE-CAR7 therapy can selectively target cancer cells, reducing the risk of harm to normal cells. This targeted approach can lead to better treatment outcomes and improved quality of life for patients.
The BE-CAR7 therapy is also a testament to the power of immunotherapy in the fight against cancer. Immunotherapy has emerged as a promising approach to cancer treatment in recent years, with several immunotherapies already approved for the treatment of various types of cancer. The BE-CAR7 therapy is an example of how immunotherapy can be used to treat aggressive blood cancers, and its success has opened up new avenues for research and development.
In conclusion, the BE-CAR7 therapy is a groundbreaking achievement that has the potential to revolutionize the treatment of T-cell acute lymphoblastic leukaemia and other types of blood cancer. The therapy’s ability to target cancer cells with high specificity and its minimal side effects make it an attractive option for patients. As research continues to advance, we can expect to see more innovative therapies emerge, giving hope to patients and their families. For more information on this breakthrough, please visit: https://www.sciencedaily.com/releases/2025/12/251211040438.htm