In a first, gene-edited cell therapy cures aggressive blood cancer
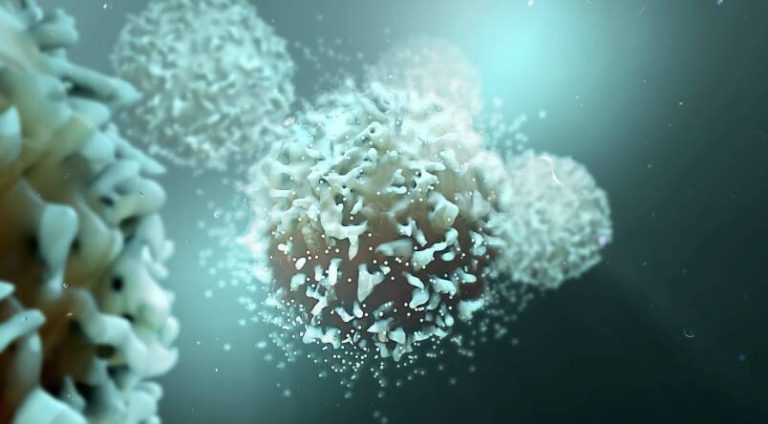
In a groundbreaking medical breakthrough, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, modifies immune cells (T-cells) to have chimeric antigen receptors (CARs) on their surface. The CARs recognize and target a specific protein on cancer cells’ surface, and the T-cell attached then destroys that cancer cell. This revolutionary approach has opened up new avenues for the treatment of aggressive blood cancers, offering hope to patients who have limited treatment options.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a type of white blood cell that plays a crucial role in the immune system. T-ALL is an aggressive disease that progresses rapidly, making it challenging to treat. Current treatment options for T-ALL include chemotherapy, radiation therapy, and bone marrow transplantation, which can have significant side effects and may not always be effective.
The BE-CAR7 therapy involves extracting T-cells from the patient’s blood and modifying them using gene editing techniques to introduce the CARs. The CARs are designed to recognize a specific protein called CD7, which is expressed on the surface of cancerous T-cells. The modified T-cells are then infused back into the patient’s body, where they can recognize and target the cancer cells, leading to their destruction.
The UK researchers conducted a clinical trial to test the safety and efficacy of the BE-CAR7 therapy in patients with T-ALL. The results were nothing short of remarkable, with all patients showing significant improvement, and some even achieving complete remission. The therapy was well-tolerated, with minimal side effects, which is a significant advantage over traditional treatments.
The BE-CAR7 therapy has several advantages over traditional treatments for T-ALL. Firstly, it is a targeted therapy, which means that it specifically targets the cancer cells, reducing the harm to healthy cells. Secondly, it is a personalized therapy, as the T-cells are extracted from the patient’s own body, reducing the risk of rejection. Finally, it has the potential to be a curative treatment, offering hope to patients who have limited treatment options.
The success of the BE-CAR7 therapy has significant implications for the treatment of aggressive blood cancers. It opens up new avenues for the development of targeted therapies that can specifically target cancer cells, reducing the harm to healthy cells. It also highlights the potential of gene editing techniques in the development of new therapies, which can be used to modify immune cells to recognize and target specific proteins on cancer cells.
The BE-CAR7 therapy is not without its challenges, however. The production of the modified T-cells is a complex and time-consuming process, which requires specialized equipment and expertise. Additionally, the cost of the therapy is likely to be high, at least in the initial stages, which may limit its accessibility to patients.
Despite these challenges, the BE-CAR7 therapy represents a significant breakthrough in the treatment of aggressive blood cancers. It offers hope to patients who have limited treatment options and highlights the potential of gene editing techniques in the development of new therapies. As research continues to advance, we can expect to see new and innovative therapies emerge, which can specifically target cancer cells, reducing the harm to healthy cells.
In conclusion, the BE-CAR7 therapy is a groundbreaking medical breakthrough that has the potential to revolutionize the treatment of aggressive blood cancers. Its success highlights the potential of gene editing techniques in the development of new therapies and offers hope to patients who have limited treatment options. As research continues to advance, we can expect to see new and innovative therapies emerge, which can specifically target cancer cells, reducing the harm to healthy cells.
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm