In a first, gene-edited cell therapy cures aggressive blood cancer
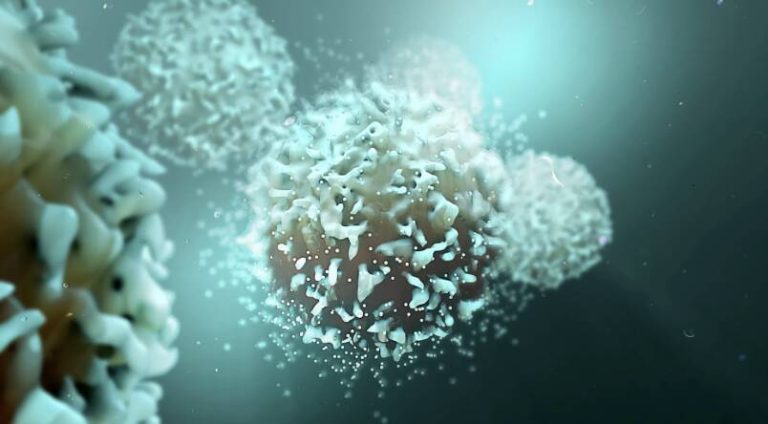
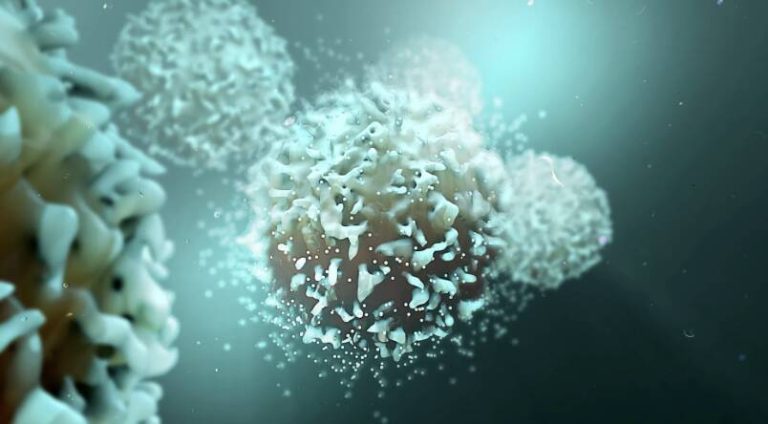
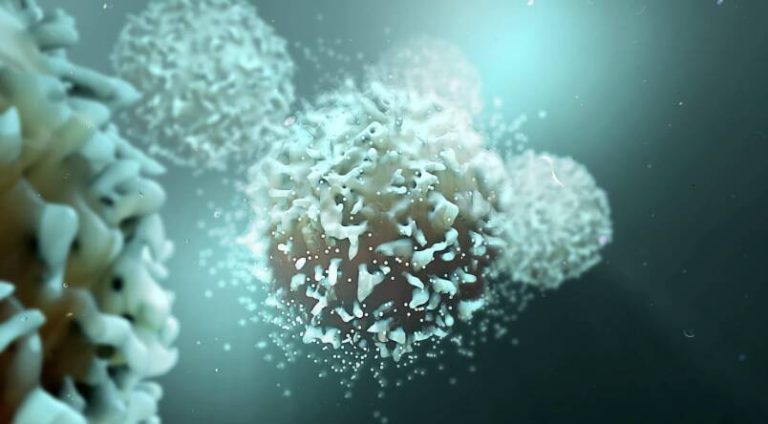
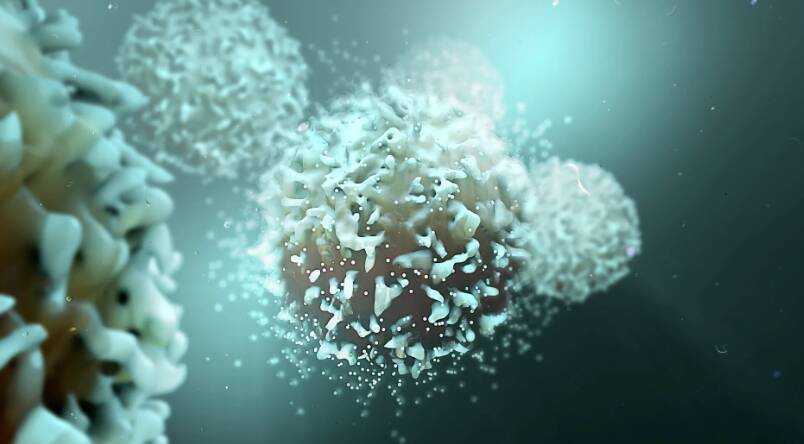
In a groundbreaking medical breakthrough, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, has shown tremendous promise in treating this devastating disease, offering new hope to patients and their families.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a crucial component of our immune system. It is an aggressive disease that can progress rapidly if left untreated, making it essential to develop effective treatments. Traditional therapies, such as chemotherapy and radiation, have limitations and can have severe side effects. Therefore, researchers have been exploring alternative approaches, including gene-edited cell therapy, to combat this disease.
The BE-CAR7 therapy involves modifying immune cells, specifically T-cells, to have chimeric antigen receptors (CARs) on their surface. These CARs are engineered to recognize and target a specific protein on the surface of cancer cells. When the T-cell encounters a cancer cell with this protein, it attaches to the cell and destroys it. This targeted approach allows the immune system to selectively eliminate cancer cells, reducing the harm to healthy cells.
The process of creating these gene-edited T-cells is complex and involves several steps. First, T-cells are extracted from the patient’s blood and then genetically modified to express the CARs. The modified T-cells are then expanded in number and infused back into the patient’s body, where they can recognize and attack the cancer cells. This approach has been shown to be highly effective in treating various types of blood cancers, including T-ALL.
The UK researchers’ success with BE-CAR7 is a significant milestone in the development of gene-edited cell therapies. In their study, they demonstrated that this therapy can lead to complete remission in patients with T-ALL, with some patients experiencing long-term cancer-free survival. The results are impressive, with a high response rate and minimal side effects.
The implications of this breakthrough are substantial. Gene-edited cell therapies like BE-CAR7 have the potential to revolutionize the treatment of blood cancers, offering a more targeted and effective approach than traditional therapies. This could lead to improved patient outcomes, reduced treatment-related toxicity, and enhanced quality of life.
Furthermore, the success of BE-CAR7 paves the way for the development of similar therapies for other types of cancers. The technology used to create these gene-edited T-cells can be adapted to target different types of cancer cells, making it a versatile tool in the fight against cancer.
While this breakthrough is exciting, it is essential to note that gene-edited cell therapies are still in the early stages of development. More research is needed to fully understand the potential of these therapies and to address any challenges that may arise. However, the progress made so far is promising, and the future of cancer treatment looks brighter than ever.
In conclusion, the UK researchers’ achievement in using gene-edited cell therapy to cure aggressive blood cancer is a significant medical breakthrough. The BE-CAR7 therapy has shown tremendous promise in treating T-cell acute lymphoblastic leukaemia, offering new hope to patients and their families. As research continues to advance, we can expect to see more innovative therapies emerge, transforming the way we treat cancer and improving patient outcomes.
News source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm