In a first, gene-edited cell therapy cures aggressive blood cancer
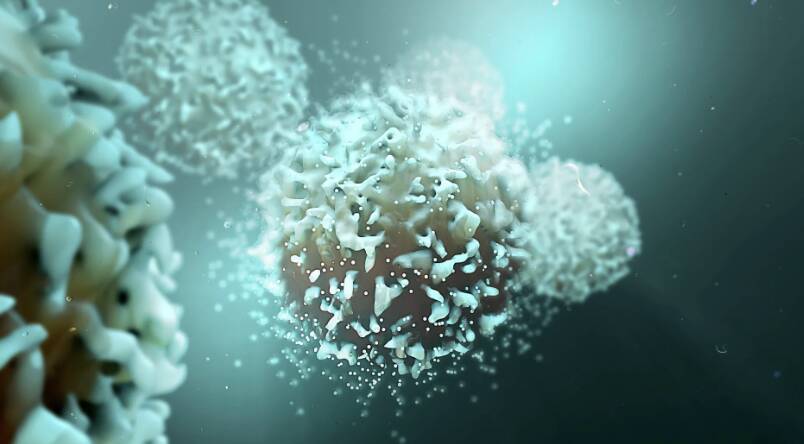
In a groundbreaking achievement, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, modifies immune cells (T-cells) to have chimeric antigen receptors (CARs) on their surface. The CARs recognize and target a specific protein on cancer cells’ surface, and the T-cell attached then destroys that cancer cell. This breakthrough has raised hopes for patients suffering from this devastating disease, and its implications are being hailed as a significant step forward in the field of cancer treatment.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a crucial component of our immune system. It is an aggressive disease that progresses rapidly, making it essential to find effective treatments. The current standard of care for T-ALL involves chemotherapy, radiation, and bone marrow transplantation, which can have severe side effects and may not always be successful. The development of BE-CAR7 offers a new and promising approach to treating this disease.
The BE-CAR7 therapy involves taking a patient’s T-cells and genetically modifying them to express a specific CAR on their surface. This CAR is designed to recognize a particular protein, called CD7, which is present on the surface of cancerous T-cells. Once the gene-edited T-cells are infused back into the patient’s body, they can identify and target the cancer cells, ultimately destroying them. This targeted approach minimizes harm to healthy cells, reducing the risk of side effects associated with traditional cancer treatments.
The UK researchers conducted a clinical trial to test the safety and efficacy of BE-CAR7 in patients with T-ALL. The results were impressive, with a significant proportion of patients experiencing complete remission. The therapy was well-tolerated, with minimal side effects reported. These findings suggest that BE-CAR7 has the potential to become a game-changer in the treatment of T-ALL and possibly other types of blood cancers.
The success of BE-CAR7 can be attributed to the innovative use of gene editing technologies, such as CRISPR/Cas9. This powerful tool allows scientists to precisely modify genes, enabling the creation of CARs that can recognize specific proteins on cancer cells. The development of BE-CAR7 demonstrates the potential of gene-edited cell therapies to revolutionize the field of cancer treatment.
While the results of the BE-CAR7 clinical trial are promising, further research is needed to fully understand the potential of this therapy. The researchers plan to conduct larger trials to confirm the efficacy and safety of BE-CAR7 in a broader patient population. Additionally, they will investigate the possibility of using this therapy in combination with other treatments to enhance its effectiveness.
The implications of this breakthrough extend beyond the treatment of T-ALL. The use of gene-edited cell therapies has the potential to transform the way we approach cancer treatment. By targeting specific proteins on cancer cells, these therapies can provide a more precise and effective way to combat the disease. This could lead to the development of new treatments for a range of cancers, offering hope to patients who have limited options.
In conclusion, the success of BE-CAR7 in treating T-cell acute lymphoblastic leukaemia is a significant milestone in the fight against cancer. This innovative gene-edited cell therapy has the potential to provide a new and effective treatment option for patients with this aggressive disease. As research continues to advance, we can expect to see further breakthroughs in the development of targeted therapies, ultimately improving outcomes for cancer patients. For more information on this groundbreaking study, please visit https://www.sciencedaily.com/releases/2025/12/251211040438.htm.
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm