In a first, gene-edited cell therapy cures aggressive blood cancer
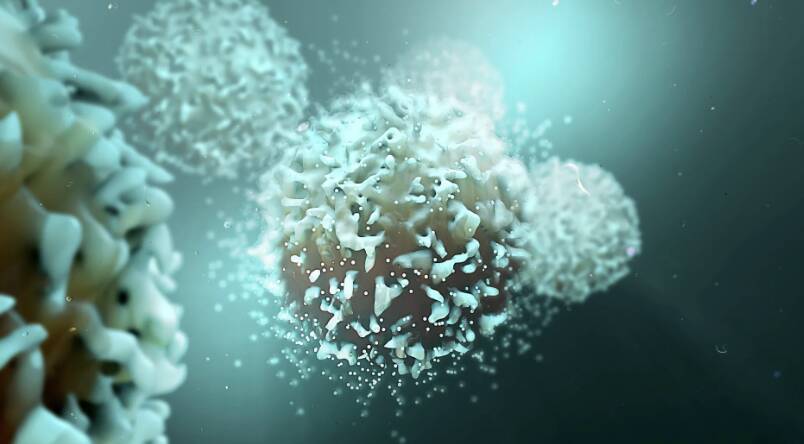
In a groundbreaking achievement, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, modifies immune cells (T-cells) to have chimeric antigen receptors (CARs) on their surface. The CARs recognize and target a specific protein on cancer cells’ surface, and the T-cell attached then destroys that cancer cell. This breakthrough has opened up new avenues for the treatment of this devastating disease, offering hope to patients and their families.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a crucial component of the immune system. It is a highly aggressive disease, with a poor prognosis, especially in adults. The current treatment options for T-ALL are limited, and the disease often relapses, making it essential to develop new and effective therapies. The BE-CAR7 therapy has shown promising results in clinical trials, with patients experiencing complete remission.
The BE-CAR7 therapy involves extracting T-cells from the patient’s blood and modifying them using gene editing techniques to introduce the CARs. The CARs are designed to recognize a specific protein, called CD7, which is present on the surface of T-ALL cancer cells. The modified T-cells are then infused back into the patient’s body, where they can recognize and target the cancer cells, destroying them. This approach has been shown to be highly effective in eliminating cancer cells, with minimal side effects.
The use of gene-edited immune cells in cancer therapy is a rapidly evolving field, with several ongoing clinical trials. The BE-CAR7 therapy is one of the first to demonstrate the efficacy of this approach in treating T-ALL. The success of this therapy can be attributed to the precision of the gene editing technique, which allows for the introduction of the CARs at a specific location in the T-cell genome. This ensures that the CARs are expressed on the surface of the T-cells, enabling them to recognize and target the cancer cells.
The BE-CAR7 therapy has several advantages over traditional cancer therapies. Firstly, it is a highly targeted approach, which reduces the risk of damage to healthy cells. Secondly, it has the potential to be more effective than traditional therapies, as it can selectively eliminate cancer cells. Finally, the use of gene-edited immune cells allows for a personalized approach to cancer therapy, where the treatment can be tailored to the individual patient’s needs.
The success of the BE-CAR7 therapy has significant implications for the treatment of T-ALL and other types of blood cancer. It offers a new hope for patients who have failed to respond to traditional therapies or have relapsed. Additionally, it has the potential to be used in combination with other therapies, such as chemotherapy and radiation, to enhance their effectiveness.
In conclusion, the BE-CAR7 therapy is a groundbreaking achievement in the field of cancer research, offering a new and effective approach to treating T-cell acute lymphoblastic leukaemia. The use of gene-edited immune cells has shown promising results in clinical trials, and this therapy has the potential to revolutionize the treatment of this devastating disease. As research continues to evolve, we can expect to see further advancements in the field of gene-edited cell therapy, offering new hope to patients and their families.
The development of the BE-CAR7 therapy is a testament to the power of collaboration and innovation in scientific research. The UK researchers who developed this therapy have made a significant contribution to the field of cancer research, and their work has the potential to benefit patients worldwide. As we continue to push the boundaries of scientific knowledge, we can expect to see further breakthroughs in the field of gene-edited cell therapy, offering new and effective treatments for a range of diseases.
In the future, we can expect to see further refinement of the BE-CAR7 therapy, with ongoing clinical trials aimed at optimizing its effectiveness and reducing its side effects. Additionally, researchers will explore the use of gene-edited immune cells in treating other types of cancer, including solid tumors. The potential of this approach is vast, and it is likely to play a major role in the development of new cancer therapies in the coming years.
As we look to the future, it is essential to recognize the importance of continued investment in scientific research. The development of the BE-CAR7 therapy is a result of years of dedicated research and collaboration, and it is a testament to the power of scientific inquiry. By continuing to support and fund scientific research, we can expect to see further breakthroughs in the field of gene-edited cell therapy, offering new hope to patients and their families.
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm






