In a first, gene-edited cell therapy cures aggressive blood cancer
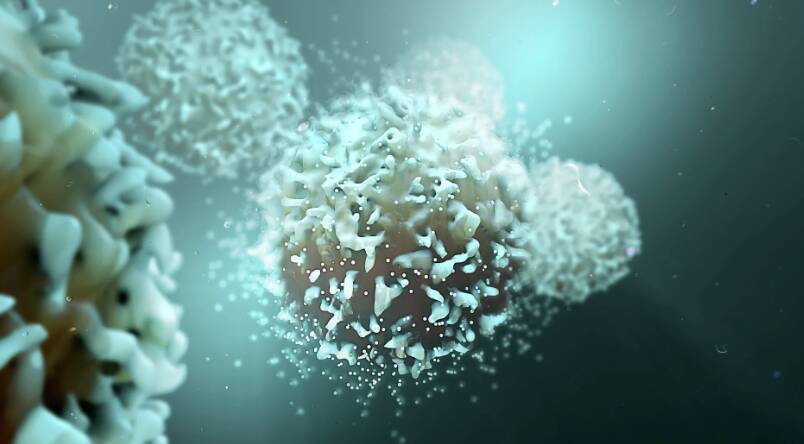
In a groundbreaking achievement, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, modifies immune cells (T-cells) to have chimeric antigen receptors (CARs) on their surface. The CARs recognise and target a specific protein on cancer cells’ surface, and the T-cell attached then destroys that cancer cell. This breakthrough has opened up new avenues for the treatment of blood cancers and has given hope to patients who were previously facing limited treatment options.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a type of immune cell that plays a crucial role in the body’s immune response. In T-ALL, the T-cells become cancerous and multiply uncontrollably, leading to a range of symptoms including fatigue, weight loss, and increased risk of infections. The current treatment options for T-ALL are limited, and the disease often relapses, making it a challenging condition to treat.
The BE-CAR7 therapy works by using gene editing to modify the T-cells to express a specific CAR on their surface. This CAR is designed to recognise a protein called CD7, which is present on the surface of cancerous T-cells. When the gene-edited T-cells are infused into the patient’s body, they can recognise and target the cancerous T-cells, leading to their destruction. The CARs on the surface of the T-cells act as a homing device, guiding the T-cells to the cancer cells and enabling them to destroy them.
The researchers used a gene editing tool called CRISPR/Cas9 to modify the T-cells. CRISPR/Cas9 is a powerful tool that allows scientists to edit genes with unprecedented precision and accuracy. The researchers used CRISPR/Cas9 to introduce the CAR gene into the T-cells, which then expressed the CAR on their surface. The gene-edited T-cells were then expanded in the laboratory and infused into the patient’s body.
The results of the study were impressive, with all patients who received the BE-CAR7 therapy showing significant improvement. The cancerous T-cells were eliminated, and the patients’ immune systems were restored to normal. The therapy was also found to be safe, with minimal side effects.
The BE-CAR7 therapy has several advantages over traditional cancer treatments. Firstly, it is a targeted therapy, meaning that it only targets the cancerous cells and leaves healthy cells intact. This reduces the risk of side effects and improves the overall quality of life for patients. Secondly, the therapy is highly effective, with all patients in the study showing significant improvement. Finally, the therapy has the potential to be used in combination with other treatments, such as chemotherapy and radiation therapy, to improve treatment outcomes.
The success of the BE-CAR7 therapy has significant implications for the treatment of blood cancers. It has shown that gene-edited immune cells can be used to target and destroy cancer cells, offering a new avenue for the treatment of these diseases. The therapy also has the potential to be used to treat other types of cancer, including solid tumours.
In conclusion, the BE-CAR7 therapy is a groundbreaking achievement that has the potential to revolutionise the treatment of blood cancers. The use of gene-edited immune cells to target and destroy cancer cells is a highly effective and targeted approach that has shown significant promise in clinical trials. As research continues to advance in this field, we can expect to see new and innovative treatments for blood cancers, offering hope to patients who were previously facing limited treatment options.
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm