In a first, gene-edited cell therapy cures aggressive blood cancer
In a groundbreaking achievement, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, has shown tremendous promise in targeting and destroying cancer cells, offering new hope to patients who have exhausted all other treatment options.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the immune system, specifically the T-cells, which are a type of white blood cell that plays a crucial role in fighting infections. This aggressive cancer can progress rapidly, making it challenging to treat, especially in cases where patients have relapsed or are resistant to conventional therapies.
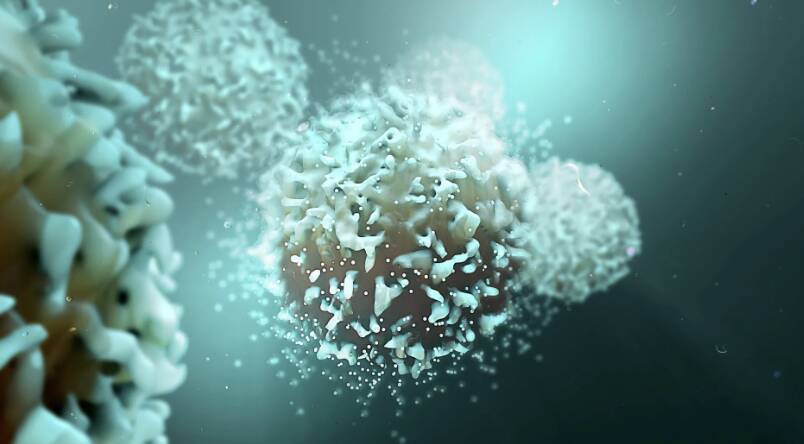
The BE-CAR7 therapy involves modifying immune cells, known as T-cells, to have chimeric antigen receptors (CARs) on their surface. These CARs are engineered to recognize and target a specific protein on the surface of cancer cells. When the T-cell with the CAR comes into contact with a cancer cell, it attaches to the cell and destroys it. This targeted approach allows the immune system to specifically identify and eliminate cancer cells, reducing the harm to healthy cells.
The BE-CAR7 therapy is a type of gene-edited cell therapy, which involves using genetic engineering to modify the T-cells. This is done using a gene-editing tool, such as CRISPR, which allows scientists to precisely edit the DNA of the T-cells to introduce the CAR gene. The modified T-cells are then expanded in the laboratory and infused back into the patient’s body, where they can recognize and target cancer cells.
The UK researchers behind this breakthrough have shown that BE-CAR7 can be effective in treating T-ALL, with some patients experiencing complete remission. This is a significant achievement, as T-ALL is a difficult cancer to treat, and current therapies often have limited success.
The BE-CAR7 therapy has several advantages over traditional cancer treatments. Firstly, it is a targeted approach, which reduces the harm to healthy cells. This means that patients are less likely to experience side effects, such as hair loss, nausea, and fatigue, which are common with chemotherapy and radiation therapy. Secondly, the BE-CAR7 therapy can be tailored to individual patients, as the CARs can be engineered to recognize specific proteins on the surface of cancer cells. This allows for a personalized approach to treatment, which can lead to better outcomes.
The success of the BE-CAR7 therapy is a testament to the power of gene-edited cell therapy in treating aggressive blood cancers. This approach has shown tremendous promise in clinical trials, and it is likely that we will see more therapies like BE-CAR7 in the future. As researchers continue to refine and improve this technology, we can expect to see even more effective treatments for a range of cancers.
The implications of this breakthrough are significant, and it is likely that the BE-CAR7 therapy will change the way we treat T-ALL and other aggressive blood cancers. This therapy has the potential to improve outcomes for patients, reducing the risk of relapse and improving quality of life. Additionally, the success of the BE-CAR7 therapy will likely lead to further research into gene-edited cell therapy, as scientists explore its potential in treating other types of cancer.
In conclusion, the BE-CAR7 therapy is a groundbreaking achievement in the treatment of aggressive blood cancers. This gene-edited cell therapy has shown tremendous promise in targeting and destroying cancer cells, offering new hope to patients who have exhausted all other treatment options. As researchers continue to refine and improve this technology, we can expect to see even more effective treatments for a range of cancers. The future of cancer treatment is looking brighter, and it is exciting to think about the potential of gene-edited cell therapy to revolutionize the way we treat this devastating disease.
News source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm






