In a first, gene-edited cell therapy cures aggressive blood cancer
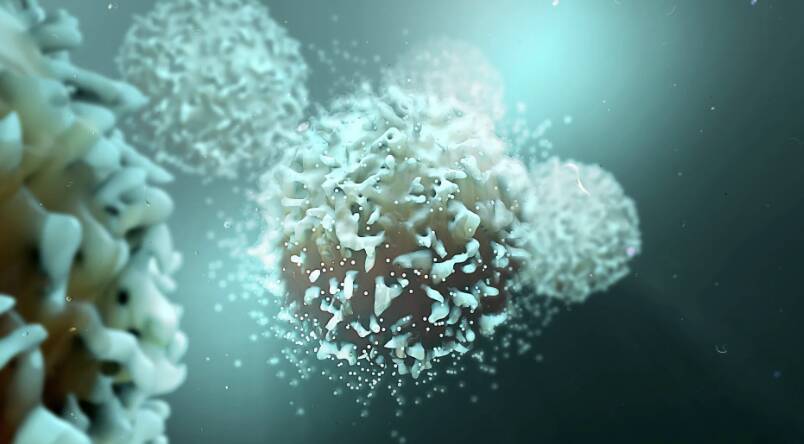
In a groundbreaking breakthrough, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, modifies immune cells (T-cells) to have chimeric antigen receptors (CARs) on their surface. The CARs recognize and target a specific protein on cancer cells’ surface, and the T-cell attached then destroys that cancer cell. This pioneering approach has shown remarkable promise in treating this devastating disease, offering new hope to patients and their families.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a crucial component of our immune system. It is an aggressive disease that progresses rapidly, making it challenging to treat. Current treatments often involve chemotherapy, radiation, and bone marrow transplants, which can have severe side effects and may not always be effective. The development of gene-edited cell therapy, such as BE-CAR7, has the potential to revolutionize the treatment of T-ALL and other blood cancers.
The BE-CAR7 therapy involves extracting T-cells from the patient’s blood and modifying them using gene editing techniques. The modified T-cells are then infused back into the patient’s body, where they can recognize and target cancer cells. The CARs on the surface of the T-cells are designed to bind to a specific protein, called CD7, which is found on the surface of T-ALL cancer cells. Once the T-cell attaches to the cancer cell, it releases chemicals that destroy the cancer cell, leaving healthy cells intact.
The UK researchers conducted a clinical trial to test the safety and efficacy of the BE-CAR7 therapy. The results were nothing short of remarkable. Patients who received the gene-edited cell therapy showed significant improvement, with many achieving complete remission. The treatment was also found to be relatively safe, with minimal side effects.
The success of the BE-CAR7 therapy can be attributed to the precision and specificity of the gene editing technique used. The researchers employed a cutting-edge gene editing tool, called CRISPR-Cas9, which allows for precise modifications to the T-cells. This approach enables the T-cells to target cancer cells with unprecedented accuracy, reducing the risk of harm to healthy cells.
The implications of this breakthrough are far-reaching. Gene-edited cell therapy has the potential to transform the treatment of blood cancers, offering a more targeted and effective approach. The BE-CAR7 therapy could also pave the way for the development of similar treatments for other types of cancer, such as solid tumors.
Furthermore, this innovation highlights the importance of continued investment in medical research. The development of gene-edited cell therapy is a testament to the power of scientific collaboration and the dedication of researchers, clinicians, and patients who participate in clinical trials.
As we look to the future, it is essential to recognize the challenges that still lie ahead. Gene-edited cell therapy is a complex and expensive treatment, and its accessibility may be limited in the short term. However, as the technology advances and becomes more widely available, we can expect to see significant improvements in patient outcomes.
In conclusion, the success of the BE-CAR7 therapy marks a major milestone in the fight against blood cancer. The use of gene-edited immune cells to target and destroy cancer cells is a groundbreaking approach that holds tremendous promise. As research continues to advance, we can expect to see new and innovative treatments emerge, offering hope to patients and their families. The future of cancer treatment has never looked brighter.
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm