In a first, gene-edited cell therapy cures aggressive blood cancer
In a groundbreaking medical breakthrough, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, has shown remarkable promise in targeting and destroying cancer cells, offering new hope for patients diagnosed with this devastating disease.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a crucial component of the immune system. It is an aggressive disease that can progress rapidly if left untreated, making it essential to develop effective treatments. Traditional therapies, such as chemotherapy and radiation, can be effective but often come with significant side effects and may not always lead to long-term remission.
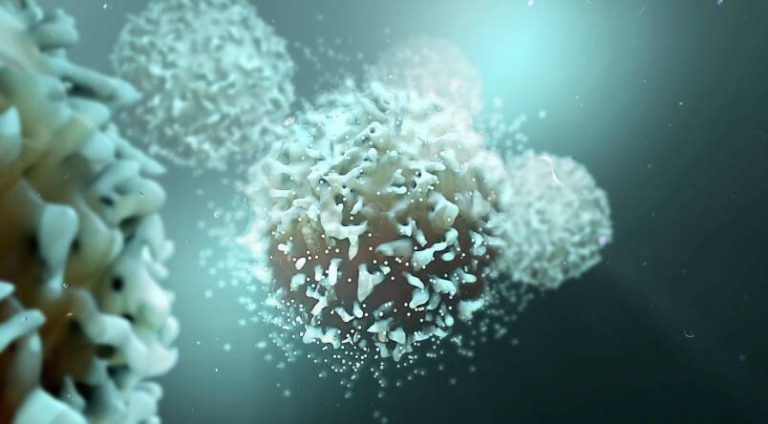
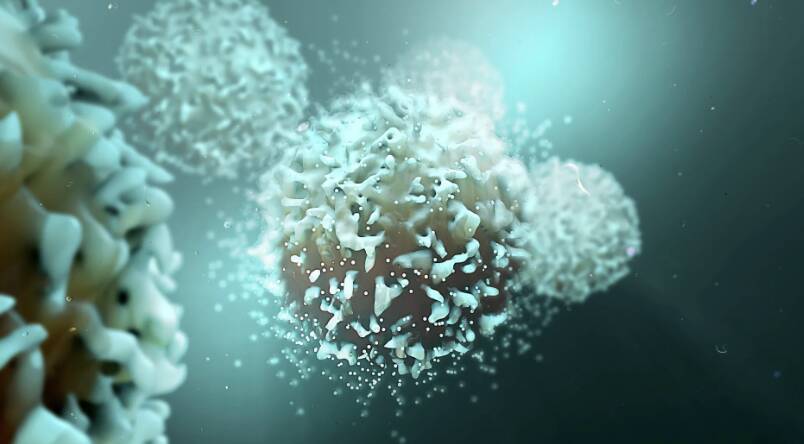
The BE-CAR7 therapy takes a different approach by harnessing the power of gene editing to modify immune cells, known as T-cells, to recognize and target cancer cells. The treatment involves removing T-cells from the patient’s blood and genetically engineering them to have chimeric antigen receptors (CARs) on their surface. These CARs are designed to recognize a specific protein on the surface of cancer cells, allowing the T-cells to identify and attach to the cancer cells.
Once the T-cells are attached to the cancer cells, they can destroy them, thereby reducing the tumor burden and preventing the progression of the disease. This targeted approach reduces the harm to healthy cells, minimizing the risk of side effects and improving the overall efficacy of the treatment.
The BE-CAR7 therapy has shown impressive results in clinical trials, with patients experiencing significant improvements in their condition. The treatment has been able to induce complete remission in some patients, offering a new lease on life for those who had limited treatment options.
The success of BE-CAR7 can be attributed to the advancements in gene editing technologies, such as CRISPR/Cas9, which have enabled researchers to precisely modify the genes responsible for the production of CARs. This has allowed for the creation of T-cells that can recognize and target specific proteins on cancer cells, making the treatment more effective and targeted.
The implications of this breakthrough are significant, and it has the potential to revolutionize the treatment of blood cancers. The BE-CAR7 therapy can be used to treat a range of blood cancers, including leukaemia, lymphoma, and multiple myeloma, offering new hope for patients who have limited treatment options.
Furthermore, the success of BE-CAR7 demonstrates the potential of gene-edited cell therapies in treating a range of diseases, including cancer, genetic disorders, and autoimmune diseases. As the technology continues to evolve, we can expect to see more innovative treatments that can target specific diseases and improve patient outcomes.
In conclusion, the development of BE-CAR7 is a significant milestone in the fight against blood cancer. This innovative therapy has shown remarkable promise in targeting and destroying cancer cells, offering new hope for patients diagnosed with T-cell acute lymphoblastic leukaemia. As research continues to advance, we can expect to see more breakthroughs in the field of gene-edited cell therapies, leading to improved treatments and better patient outcomes.
The future of cancer treatment is looking brighter, thanks to the dedication and hard work of researchers and scientists who are pushing the boundaries of medical innovation. As we continue to explore the potential of gene-edited cell therapies, we can expect to see more exciting developments in the years to come.
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm