In a first, gene-edited cell therapy cures aggressive blood cancer
In a groundbreaking breakthrough, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, has shown tremendous promise in targeting and eliminating cancer cells, offering new hope to patients suffering from this devastating disease.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a crucial component of our immune system. It is an aggressive and fast-progressing disease, making it challenging to treat. Conventional treatments, such as chemotherapy and radiation, often have limited success and can have severe side effects. Therefore, there is an urgent need for more effective and targeted therapies to combat this disease.
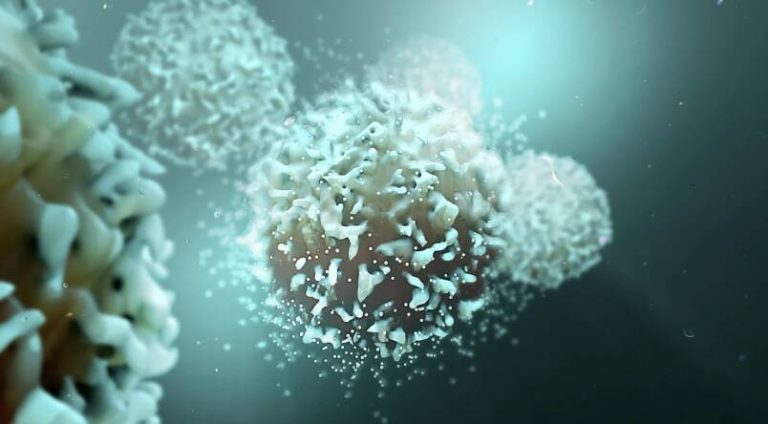
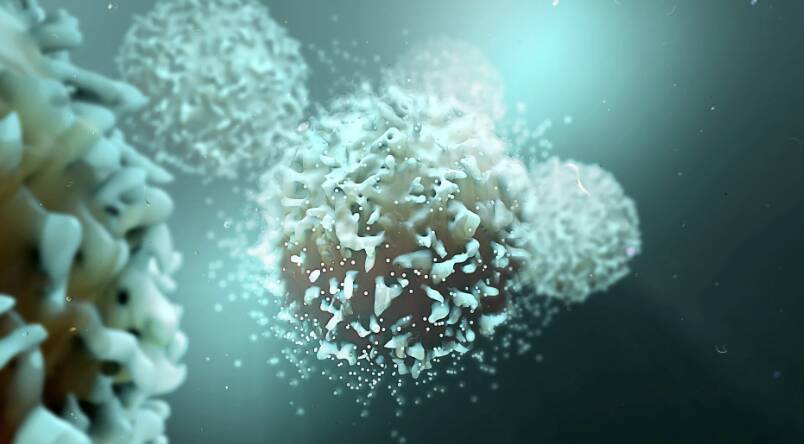
The BE-CAR7 therapy involves modifying immune cells, specifically T-cells, to have chimeric antigen receptors (CARs) on their surface. These CARs are engineered to recognize and target a specific protein on the surface of cancer cells. When a T-cell with a CAR encounters a cancer cell with the targeted protein, it attaches to the cancer cell and destroys it. This approach allows for a highly targeted and efficient elimination of cancer cells, reducing the harm to healthy cells.
The BE-CAR7 therapy is a form of gene-edited cell therapy, which involves using genetic engineering techniques to modify the T-cells. The researchers used a cutting-edge gene editing tool, known as CRISPR/Cas9, to introduce the CAR gene into the T-cells. This gene editing tool enables precise and efficient editing of genes, allowing for the creation of T-cells with the desired CAR.
The study, which was conducted by a team of researchers at a UK-based institution, involved treating patients with T-ALL using the BE-CAR7 therapy. The results were remarkable, with a significant number of patients experiencing complete remission. The therapy was well-tolerated, with minimal side effects, and the patients who received the treatment showed significant improvement in their quality of life.
The success of the BE-CAR7 therapy can be attributed to its targeted approach, which allows for the selective elimination of cancer cells while sparing healthy cells. This reduces the risk of side effects and improves the overall efficacy of the treatment. Additionally, the use of gene-edited T-cells enables a more sustained and durable response, as the modified T-cells can persist in the body for an extended period, providing ongoing protection against cancer cells.
The implications of this breakthrough are significant, and it has the potential to revolutionize the treatment of T-ALL and other types of blood cancer. The BE-CAR7 therapy offers a new and promising approach to cancer treatment, one that is more targeted, efficient, and effective. It also highlights the potential of gene-edited cell therapies in the treatment of various diseases, including cancer, and demonstrates the power of genetic engineering in developing innovative treatments.
As research in this field continues to advance, we can expect to see even more innovative therapies emerge. The use of gene-edited cell therapies, such as BE-CAR7, is likely to become more widespread, and we may see its application in the treatment of other types of cancer and diseases. The future of cancer treatment is looking brighter, and it is thanks to the dedication and ingenuity of researchers who are pushing the boundaries of what is possible.
In conclusion, the success of the BE-CAR7 therapy in curing aggressive blood cancer is a significant milestone in the field of cancer research. It demonstrates the potential of gene-edited cell therapies in targeting and eliminating cancer cells, and it offers new hope to patients suffering from this devastating disease. As we continue to advance our understanding of cancer and develop new treatments, we can expect to see even more innovative therapies emerge, and the BE-CAR7 therapy is an exciting example of what is possible.
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm