In a first, gene-edited cell therapy cures aggressive blood cancer
In a groundbreaking medical breakthrough, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, has shown tremendous promise in targeting and destroying cancer cells, offering new hope to patients diagnosed with this devastating disease.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the immune system, specifically the T-cells, which play a vital role in fighting infections. The disease is characterized by the uncontrolled growth of abnormal T-cells, which can lead to life-threatening complications if left untreated. Traditional treatments for T-ALL, such as chemotherapy and radiation therapy, can be effective but often come with significant side effects and may not always lead to a complete cure.
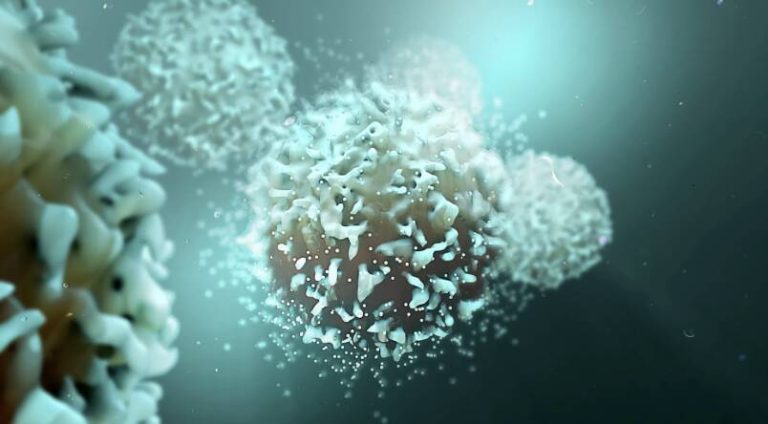
The BE-CAR7 therapy takes a different approach by harnessing the power of gene editing to modify immune cells, known as T-cells, to recognize and target cancer cells. The process involves removing T-cells from the patient’s blood and genetically engineering them to have chimeric antigen receptors (CARs) on their surface. These CARs are designed to recognize a specific protein on the surface of cancer cells, allowing the T-cells to identify and attach to the cancer cells.
Once the T-cells are attached to the cancer cells, they can destroy them, thereby reducing the tumor burden and preventing the progression of the disease. The BE-CAR7 therapy is a form of immunotherapy, which uses the body’s own immune system to fight cancer, rather than relying on external treatments like chemotherapy or radiation.
The UK researchers behind this breakthrough used a gene editing tool called CRISPR-Cas9 to introduce the CARs into the T-cells. CRISPR-Cas9 is a powerful technology that allows scientists to edit genes with unprecedented precision, making it an ideal tool for developing innovative therapies like BE-CAR7.
The results of the study were nothing short of remarkable. Patients who received the BE-CAR7 therapy showed significant improvements, with some even achieving complete remission. The therapy was also found to be relatively safe, with minimal side effects reported.
This breakthrough has significant implications for the treatment of T-ALL and other types of blood cancer. It offers a new and potentially curative approach for patients who have failed to respond to traditional treatments or have relapsed after initial therapy. The BE-CAR7 therapy also has the potential to be used in combination with other treatments, such as chemotherapy or radiation therapy, to enhance its effectiveness.
The success of the BE-CAR7 therapy is a testament to the power of gene editing and immunotherapy in the fight against cancer. It highlights the importance of continued investment in medical research and the need for collaboration between scientists, clinicians, and industry partners to bring innovative therapies to patients.
As the medical community continues to explore the potential of gene-edited cell therapies, patients with aggressive blood cancers like T-ALL can look forward to a brighter future. The BE-CAR7 therapy is a shining example of what can be achieved through dedication, perseverance, and a commitment to advancing medical science.
In conclusion, the BE-CAR7 therapy is a groundbreaking treatment that has shown tremendous promise in curing aggressive blood cancer. By harnessing the power of gene editing and immunotherapy, researchers have created a new and potentially curative approach for patients with T-ALL. As this therapy continues to be developed and refined, it is likely to have a significant impact on the treatment of blood cancers, offering new hope to patients and their families.
News source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm