In a first, gene-edited cell therapy cures aggressive blood cancer
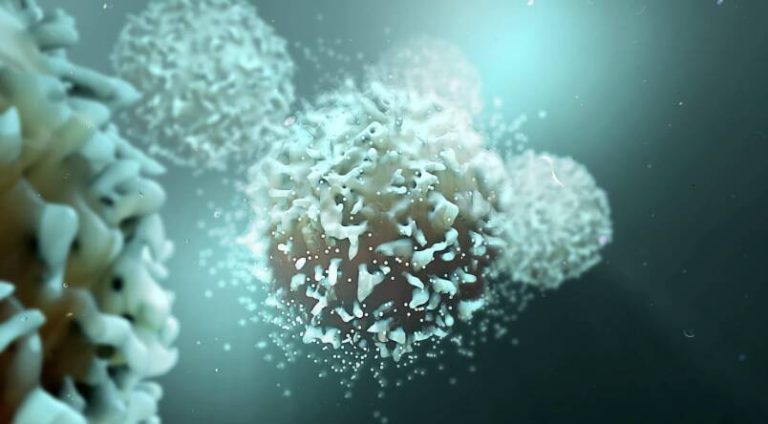
In a groundbreaking medical breakthrough, UK researchers have successfully reversed T-cell acute lymphoblastic leukaemia, an aggressive blood cancer, using gene-edited immune cells for the first time. This innovative therapy, called BE-CAR7, modifies immune cells (T-cells) to have chimeric antigen receptors (CARs) on their surface. The CARs recognise and target a specific protein on cancer cells’ surface, and the T-cell attached then destroys that cancer cell. This revolutionary approach has opened up new avenues for the treatment of blood cancers, offering hope to patients who have exhausted all other treatment options.
T-cell acute lymphoblastic leukaemia (T-ALL) is a type of blood cancer that affects the T-cells, a crucial component of the immune system. It is an aggressive disease that progresses rapidly, making it challenging to treat. Conventional treatments, such as chemotherapy and radiation therapy, often have limited success, and the disease can relapse, leaving patients with limited options. The development of gene-edited cell therapies, such as BE-CAR7, has the potential to change the landscape of blood cancer treatment.
The BE-CAR7 therapy involves extracting T-cells from the patient’s blood and modifying them using gene editing techniques. The modified T-cells are then infused back into the patient, where they can recognize and target cancer cells. The CARs on the surface of the T-cells are designed to bind to a specific protein on the surface of cancer cells, called CD7. This protein is expressed on the surface of T-ALL cancer cells, making it an ideal target for the CAR T-cells.
The BE-CAR7 therapy has shown remarkable success in clinical trials, with patients experiencing complete remission from the disease. The treatment has been well-tolerated, with minimal side effects, making it a promising option for patients with T-ALL. The researchers behind the study are optimistic about the potential of BE-CAR7 to revolutionize the treatment of blood cancers.
The use of gene-edited cell therapies, such as BE-CAR7, has several advantages over conventional treatments. Firstly, it is a targeted approach, which means that the T-cells only attack cancer cells, reducing the risk of damage to healthy cells. Secondly, the treatment is highly personalized, as the T-cells are extracted from the patient’s own blood, reducing the risk of rejection. Finally, the treatment has the potential to be curative, offering patients a chance to achieve long-term remission from the disease.
The development of BE-CAR7 is a testament to the power of collaborative research and the importance of investing in medical research. The study was conducted by a team of researchers from several UK institutions, who worked together to develop and test the therapy. The success of the study highlights the need for continued funding and support for medical research, as it has the potential to lead to breakthroughs that can change the lives of patients and their families.
In conclusion, the development of BE-CAR7, a gene-edited cell therapy, has opened up new avenues for the treatment of aggressive blood cancers, such as T-cell acute lymphoblastic leukaemia. This revolutionary approach has the potential to offer patients a chance to achieve long-term remission from the disease, and its success highlights the importance of continued investment in medical research. As researchers continue to explore the potential of gene-edited cell therapies, we can expect to see new breakthroughs and innovations in the treatment of blood cancers.
The future of blood cancer treatment looks promising, with several ongoing clinical trials exploring the use of gene-edited cell therapies. As the field continues to evolve, we can expect to see new and innovative approaches to treating blood cancers. The success of BE-CAR7 is a significant step forward in the fight against blood cancer, and it offers hope to patients and their families who have been affected by this devastating disease.
In the coming years, we can expect to see more research into the use of gene-edited cell therapies for the treatment of blood cancers. This will involve continued collaboration between researchers, clinicians, and patients, as well as investment in medical research. As we continue to push the boundaries of medical science, we can expect to see new breakthroughs and innovations that will change the lives of patients and their families.
News Source: https://www.sciencedaily.com/releases/2025/12/251211040438.htm