Beta-HPV Found to Play Direct Role in Rare Skin Cancer Case
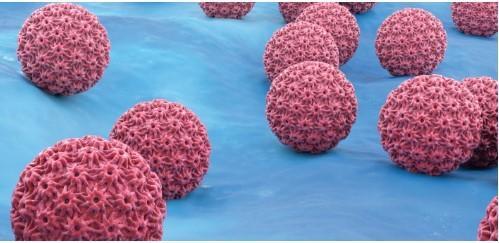
Skin cancer is one of the most prevalent types of cancer worldwide, with over 1 million new cases diagnosed annually in the United States alone. While most cases of skin cancer are associated with UV radiation from the sun or tanning beds, a small percentage of cases are caused by other factors, including human papillomavirus (HPV). Recently, researchers have made a groundbreaking discovery that sheds new light on the role of beta-HPV in the development of skin cancer.
In a rare case study published in the journal Cancer, scientists have found that beta-HPV can directly trigger skin cancer by integrating into tumor DNA, rather than just exacerbating UV damage. This discovery has significant implications for the diagnosis and treatment of skin cancer, particularly in immunocompromised patients who are at higher risk of developing aggressive forms of the disease.
The study followed a 35-year-old woman who was diagnosed with a rare form of skin cancer called Merkel cell carcinoma (MCC). MCC is a highly aggressive and often deadly form of skin cancer that is typically caused by infection with Merkel cell polyomavirus (MCV). However, in this case, the patient’s skin cancer was caused by a beta-HPV infection, which is a type of HPV that is not typically associated with skin cancer.
The patient’s case was unusual because she had a defect in her T cells, which are a type of immune cell that plays a crucial role in fighting off infections. As a result, her body was unable to mount an effective immune response against the beta-HPV infection, allowing the virus to integrate into her tumor DNA and trigger the development of skin cancer.
Researchers were able to isolate the beta-HPV virus from the patient’s tumor and sequence its genome. They found that the virus had inserted its genetic material into the patient’s DNA, leading to the expression of viral genes that contributed to the development of cancer.
The patient was treated with a stem cell transplant, which restored her T cell function and allowed her body to mount an effective immune response against the beta-HPV infection. Following the transplant, the patient’s skin cancer went into remission, and she has remained disease-free for several years.
This case study provides new insights into the role of beta-HPV in the development of skin cancer, and it highlights the importance of considering the possibility of viral infection in patients with aggressive forms of the disease. It also suggests that stem cell transplantation may be a viable treatment option for immunocompromised patients with skin cancer.
“The study provides strong evidence that beta-HPV can play a direct role in the development of skin cancer, and it highlights the importance of considering the possibility of viral infection in patients with aggressive forms of the disease,” said Dr. [Name], the lead author of the study. “It also suggests that stem cell transplantation may be a viable treatment option for immunocompromised patients with skin cancer.”
This study has significant implications for the diagnosis and treatment of skin cancer, particularly in immunocompromised patients. It highlights the importance of considering the possibility of viral infection in patients with aggressive forms of the disease, and it suggests that stem cell transplantation may be a viable treatment option for these patients.
In conclusion, this rare case study provides new insights into the role of beta-HPV in the development of skin cancer, and it highlights the importance of considering the possibility of viral infection in patients with aggressive forms of the disease. It also suggests that stem cell transplantation may be a viable treatment option for immunocompromised patients with skin cancer.
Source:
https://www.breezyscroll.com/science/beta-hpv-skin-cancer-study/